Potential Emergency Department Code Changes Due to COVID-19 Pandemic
By David Bujeda, Senior Architectural Job Captain at BAM Creative, New York
Emergency Departments have been part of the frontline response to the pandemic since the beginning of the virus outbreak. The evolving crisis meant more people confined to home while testing, albeit insufficient, was developed. Any given Emergency Department facility needed to change protocols every day. The evolution of the pandemic during the last year brought up the question of how future Emergency Department needs to be adaptable and responsive to different scenarios, considering that these areas are already the most stressful, versatile, and dynamic in a healthcare facility.
Architects, engineers, and healthcare providers needed to identify strategies to consider the worst-case scenarios. It is vital to rethink flexible spaces and mechanical parameters, with most of the spaces and systems being adaptable to meeting evolving situations and guaranteeing safety of the staff, visitors, and patients.
With these premises, we could divide and list the code regulations that need to be reviewed considering these present and future scenarios in three chapters. The first parameters to be redefined would be the safety protocols, which are the initial responses from the hospital staff to react in the event of a pandemic. In conjunction with that, architectural code changes and new requirements would need to be implemented in advance to make the first approach more effective by directing the patients to designated areas in a safe way. The last, and very important with airborne diseases from a mechanical (HVAC) standpoint view: segregating and isolating specific areas to treat infected patients to prevent the transmission to the rest of the facility and maintain a shielded environment.
Safety Protocols
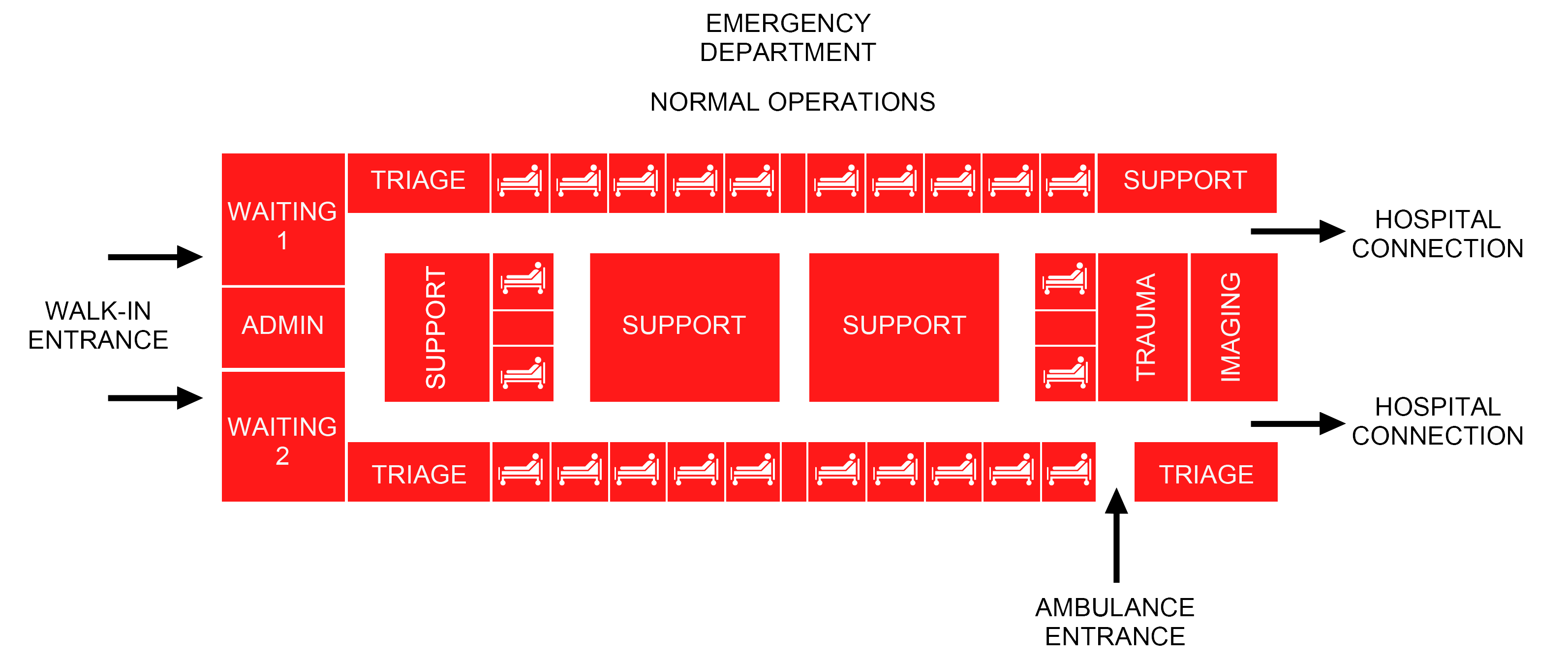
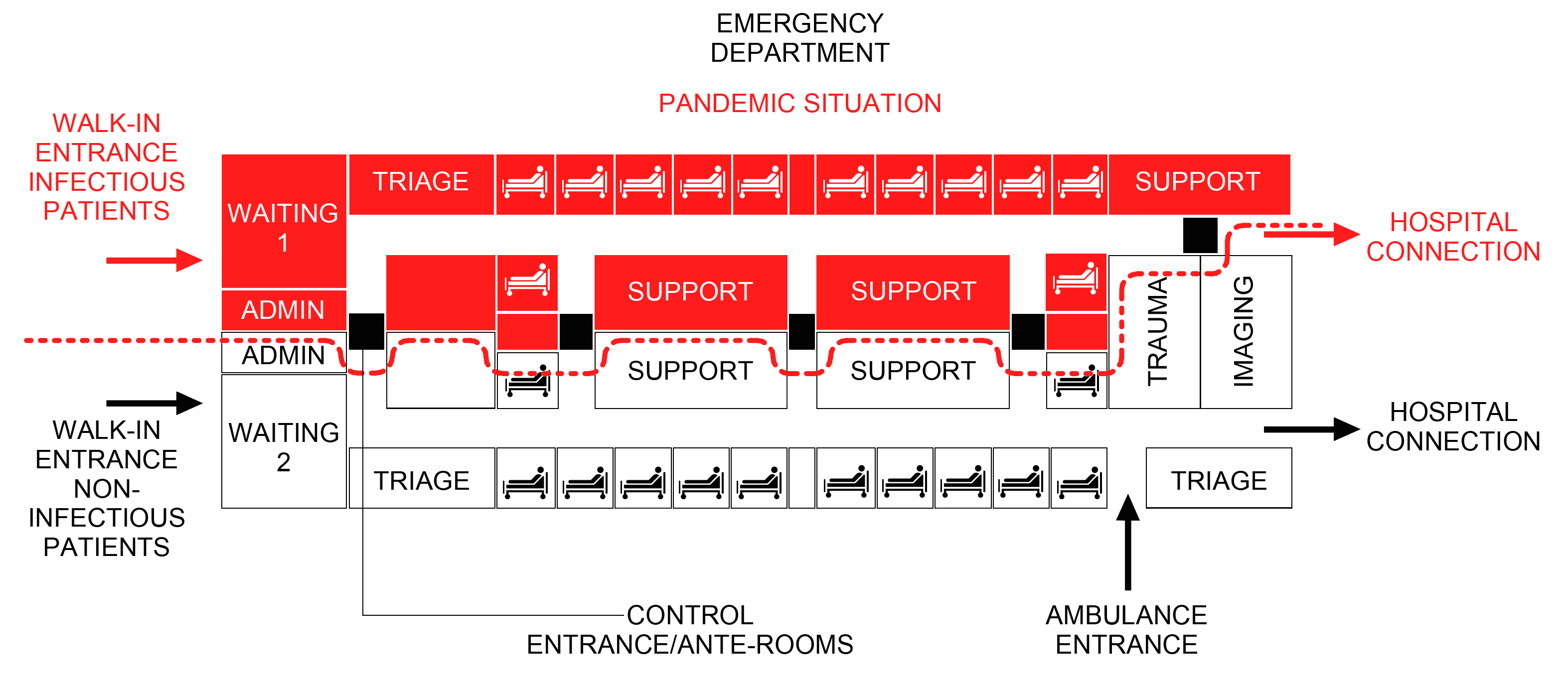
Emergency response workers are more than familiar with safe work practices and standard precautions to prevent the transmission of infectious diseases, and that includes close coordination and effective communication. Diverting infectious patients to the appropriate intake space, separately from the emergency and walking wounded is critical and the most effective protocol to navigate through airborne pandemics. Therefore, the first space to be redesigned would in this case be the waiting rooms. Reconfigure the Emergency Department seating areas to guarantee social distance between patients with Covid symptoms shall include safety seating arrangements, dividers, differentiation of travel paths, signage, etc. Rather than expanding waiting areas, infectious and non-critical patients can be diverted elsewhere in the system, as an example of flexible spaces, but always keeping in mind that all the tasks shall be performed in areas specifically designated for this purpose.
Patient Policies will need code revisions to request patients and visitors to have masks or face covering ad minimum. Dispensing machine areas shall be included when designing these spaces, in addition to handwashing stations, gloves boxes, hand sanitizers, etc. These Disinfection Stations shall be clearly marked separately for patients and staff members.
On the other hand, where technology is involved, the industry and manufacturers have a variety of tools that can work in conjunction with human-related policies to mitigate, reduce or eliminate the transmission of airborne diseases. This should take into consideration that this type of virus or bacteria can be spread not only through respiratory droplets, but also by touching surfaces contaminated by infected patients. Devices connected to occupancy sensors (thermal and movement) such as UV disinfection lighting for specific rooms (toilets, elevators, soiled or clean rooms, exam rooms, triage, gown areas, etc.), or combo UV/HEPA light ceiling mounted, or self-cleaning toilets, or movable Ultraviolet-HEPA-Carbon-Photocatalysis air purification systems units (on demand) for rooms that require decontamination protocols, shall be part of the new requirements when analyzing/designing new facilities or renovating existing ones. Some of this equipment can be used during off-business hours throughout the facility, hence new spaces for storing or increasing the sizes currently required by code shall be reviewed; training for facilities personnel shall be incorporated in their responsibilities.
Architectural Code Changes And New Requirements
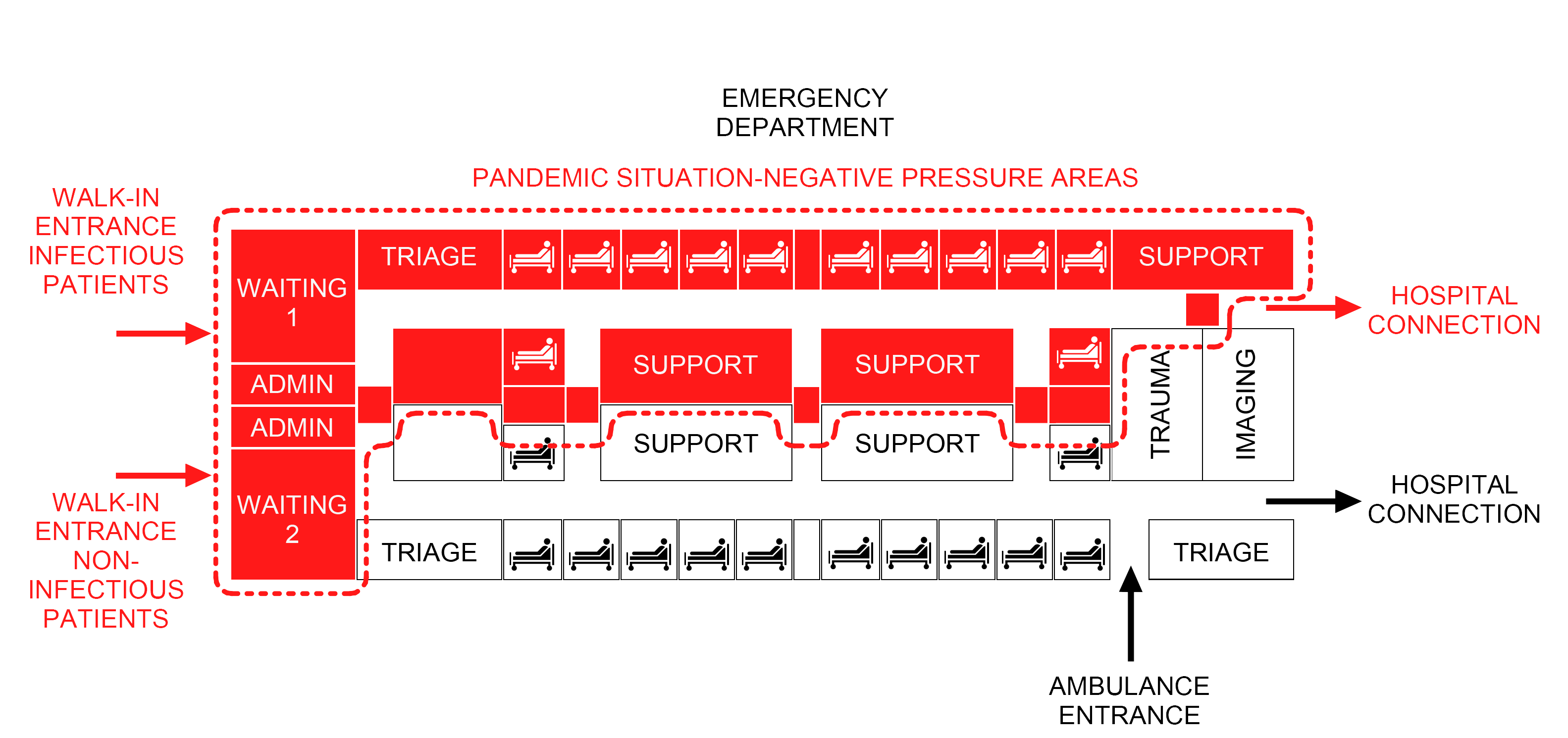
It is well known that the first contact that the patient has in a hospital in the event of an emergency is with the check-in/control desks or the waiting areas as we mentioned above, and the architectural code revisions shall begin at these starting points where the infectious patient arrives at the facility. Code regulations shall examine the potential transformation of these rooms to be divided with infectious patients and noninfectious patients, including separate entrances, temporary physical divisions (walls or glass partitions, individual pods, etc.). Associated with these large spaces are the support rooms that could be dedicated to patients with different symptomatology, even if this means duplicating the number of rooms required for the same purpose (toilets, triage rooms, soiled rooms, etc.), and always considering and evaluating the dimensions of the facility to be designed.
Since the only way to determine that a patient has specific symptomatology associated with an airborne disease is to analyze samples, collecting booths might be required for that purpose to divert the patients to the designated waiting area or exam room in time of pandemic. Within this effort to reduce the crossing between infectious patient and others with different symptomatology, distinct paths of travel shall be drawn up, including corridors, elevators, stairs, and access to other areas of the facility.

Once evaluated the changes in the above-mentioned spaces, we can focus on the restricted areas where patients are escorted by staff members. These spaces shall be then segregated for this infrequently-occurring situation and temporary control or checkpoints shall be designed to prevent disease outbreaks (in fully restricted areas) where the staff can gown, decontaminate, dispose soiled PPE, or even take a shower. A good location for these check points can be the corridors that connect different areas in the Emergency Department. These temporary spaces therefore shall be negatively pressurized, with the same parameters for air quality/renovation as others required by code in the facility.
As we move forward in this evaluation and code change requirements, dedicated rooms that support these facilities shall be specifically designated for pandemic scenarios or other mass casualty events. This shall include general or equipment storage rooms, soiled rooms, janitor closets, stretchers alcoves and, of course, not limited to any other soft/ancillary workspace, such as tele-health consultation, reading rooms, offices, etc. Other areas, such as decontamination rooms, critical to navigating unique circumstances shall be included to review protocols and spaces should be designated specifically for decontamination of respirators, reusable PPE, and miscellaneous or reusable medical equipment (stethoscopes, blood pressure cuffs, etc.).
But we should not reduce our response, analysis, and changes inside the physical and architectural volume of the Emergency Department.
If the number of infectious patients is increasing and the campus or vicinity streets allow temporary and adjacent expansion of the Emergency Department in times of pandemic, like a field hospital with a dedicated area for this purpose including the minimal rooms listed to run these short-term areas, the code shall include a chapter to determine the requirements for this specifics. In addition to this, as we learned through various responses around the world, drive-through testing spaces can be designed to avoid a mass of patients waiting to be tested inside the Emergency Department.
While we are not limiting the new code requirements to architectural aspects inside the facilities, we need to acknowledge that more and more demanded devices can reduce the transmission of virus and bacteria with ‘passive’ human actions. This is an aspect that has been evaluated by different entities and the industry to help patients and staff to have easy access, but now they are becoming more popular because of the pandemic. For instance, including automatic operators and motion/wave sensors on doors, foot/voice-operated controls on elevators, wave card readers, or any touchless devices (hand sanitizer stations, faucets, paper towel or soap dispensers in toilets or amenity bars, etc.), shall be listed in the code to prevent and reduce disease transmission. Undoubtedly, more technology would be involved, but that we can categorize under the MEP changes as defined below.
Summary Diagrams For Emergency Departments
HVAC Code Changes and New Requirements
Ventilation and filtration can reduce the airborne concentration of the virus and thus the risk of transmission through air. Promoting healthy air quality in spaces and facilities is part of the effort from the engineering community and building operations. The Center for Disease Control (CDC) has determined that COVID-19 is transmitted through two principal means: person to person and surface transmission. Engineers should focus their work on the HVAC systems to make them more efficient to prevent virus spread through sneezing, coughing, or speaking (person to person contact). Attention should also be paid to maintaining adequate air velocity, humidity and filtration systems to explore new paths, demanding new code changes and requirements to adapt the HVAC to these exceptional situations. ASHRAE is one of the best resources that give some guidance to accomplish these changes in the mechanical systems and is actively seeking solutions for future mitigation of the transmission of pathogens through the air. As stated by the ASHRAE, “Unconditioned spaces can cause thermal stress to people that may be directly life threatening and that may also lower resistance to infection.”
According to the 2018 FGI and ANSI/ASHRAE/ASHE Standard 170-2017, there is a list of rooms that should be negatively pressurized in Emergency Departments including but not limited to: waiting areas, decontamination and triage rooms, bathrooms, soiled workrooms or soiled holding rooms, janitors closets, and airborne infection isolation (AII) rooms, etc.
For new projects, the code shall consider the increase of areas with negative pressure and exhaust capability, given the architectural parameters and the flexible areas analyzed in the preceding sections. In this case, the code shall contemplate two scenarios: normal operations, with the system running with the minimum requirements; pandemic mode/exceptional operations, with the system modified to add areas to negative pressure and accommodate the spaces to the new code requirements to guarantee 100% ventilation from these areas.
From a mechanical standpoint, enhancing air filtration systems with filters, including MERV rating capable of filtering Covid-19 particles such as HEPA filters, or increasing the minimum outdoor air damper settings with natural air when possible shall be a revision to be considered by the authorities.
Conclusion
It has been a long year of both trauma and resilience since the start of the global Covid-19 pandemic. The virus disrupted our lives, transformed our workplaces, modified our human/social interactions, and furthermore, the hospitals and healthcare facilities needed to adapt their spaces to avoid being overwhelmed with patients as the cases rose every day, outfitting more and more areas to negative pressure so contaminated air could not escape. Protocols were changed daily. We all just received snapshots of stressful situations, while healthcare providers were devastated, experiencing pandemic fatigue under wretched working conditions, families were struggling and losing loved ones, virtually all businesses were shut down.
But still, in some aspects related to code regulations and future changes, there is a long path to make the right revisions and implement those modifications once all the parties receive and analyze all the data and reach an agreement for future events like this one. Changes in architecture and code are slow, but there is hope in the healthcare sector to get together, involve all the active agents (architects, engineers, AHJ, etc.), leave the trench behind and work diligently to provide better protocols, adaptable spaces and mechanical systems adjustable to different scenarios in the future. Healthcare workers made a colossal effort and it is time to listen to their demands and envision new architecture for hospitals of the future, not only the Emergency Departments.
Sources
https://www.chthealthcare.com/blog/negative-pressure-rooms
https://www.hfmmagazine.com/articles/3841-ashe-issues-covid-19-advisory-for-facilities-managers
https://www.amitahealth.org/covid-19/emergency-department
https://www.cdc.gov/hai/prevent/infection-control-assessment-tools.html
https://www.cdc.gov/coronavirus/2019-ncov/hcp/ways-operate-effectively.html
https://covid-19.uwmedicine.org/Pages/default.aspx
https://www.ashrae.org/technical-resources/resources
https://www.ashrae.org/file%20library/technical%20resources/covid-19/eiband-airbornetransmission.pdf